Residency Program

Family Medicine Residency Program
We prepare full-spectrum family physicians from a wide range of backgrounds, dedicated to the delivery of exceptional care to all, to provide family-centered, community-responsive care that addresses community needs and advances health outcomes for all.
Since 1972, the Department of Family and Community Medicine has been providing excellence in resident training. We have one ACGME-accredited family medicine program with two separate and unique tracks, each named for the location of their continuity clinic experience.
- Alvernon, which focuses on the Tucson community and surrounding areas
- South Campus, which emphasizes rural practice and includes required rural rotations (approximately 16 weeks throughout the three years with no more than three weeks away from Tucson at a time). Travel and lodging is funded by a grant from the Arizona Area Health Education Center.
Our innovative 2+2 program structure for both of our tracks allows residents to have foundational inpatient experiences caring for hospitalized adults, children and maternity patients, coupled with immersive experiences in the outpatient center to build a robust continuity panel in the office. Our curriculum is guided by residents’ feedback and experiences and is designed to provide the knowledge and skills necessary to provide culturally competent care to our diverse patients across their lifespans.
Both tracks share a core set of values:
- Commitment to excellence in education and clinical care, providing rigorous and well-rounded experiences
- Commitment to creating a sustainable, adaptable and inclusive learning environment
- Commitment to serving the needs of the communities of Arizona, especially the those that have been historically marginalized
If you want to apply to both tracks, you must select each track separately under the Program Name: University of Arizona College of Medicine – Tucson Program.
To accomplish our mission, we:
- Provide robust and comprehensive training to enable residents to be proficient in inpatient and outpatient medicine to serve individuals of all ages.
- Foster an educational environment that allows residents to build their unique identity as family physicians with an emphasis on personal growth and well-being.
- Provide individuals with opportunities for longitudinal training experiences in community medicine, rural medicine and refugee care using a holistic approach to gain an appreciation of the unique needs of their community, medically underserved and marginalized populations.
- Train individuals to be competent in the breadth of the family medicine scope of practice.
- Provide educational role models from a wide variety of backgrounds and varied practices of family medicine to educate residents on the development of life-long skills that they will use throughout their career.
Program Highlights
- As part of our curriculum, we have longitudinal threads on resident well-being and resiliency, point of care ultrasound (POCUS), health care disparities and advocacy, as well as quality improvement and patient safety.
- We offer the option to apply for distinction tracks in community medicine, Spanish language and health care disparities, and global health.
- Residents in our program receive training in integrative medicine through participation in the longitudinal Integrative Medicine in Residency curriculum. Our program weaves these concepts of integrative medicine into our mission of working with underserved populations through our clinical care.
- Family medicine faculty take the principal role in teaching clinical and academic skills, encouraging the development of lifelong skills needed to balance professional and personal roles, and fostering the realization of one’s unique identity as a family physician.
- Our program supports resident involvement in various community projects, and nurtures an enjoyable, respectful and supportive environment.
Curriculum

Our program is one of only 25 family medicine residency programs nationwide that has been granted a waiver to allow us to explore innovative residency scheduling structures.
In 2018, we implemented a “2+2” rotation structure. This change focused our residents’ clinical experience on foundational inpatient experiences with equal focus on the outpatient family medicine practice. Residents alternate between two weeks of non-family medicine clinic work and two weeks of outpatient work in the family medicine center, managing their continuity panel.
These changes have resulted in regular resident presence in the family medicine center to facilitate patients’ access to care, close working relationships within our clinic teams and improved preparation for residency graduates to lead interdisciplinary teams.
Example of a block schedule from each track:

click on image to enlarge

Didactic Day
Our didactic sessions take place during protected time every Thursday afternoon. We have a robust curriculum adapted from the Family Medicine Residency Curriculum Resource (RCR) list of high-yield topics and specifically applied to the needs and requests of our residents. The overarching goal of our didactic sessions is to ensure that we graduate capable and knowledgeable family physicians, which is done through a variety of engaging and interactive instruction sessions including resident/faculty topic reviews, Journal Club, Evidence Based Medicine Session, M&Ms, guest lecturers from the university system and surrounding community, integrative medicine sessions, as well as a variety of practice management/QI sessions to provide our residents with additional skill sets in these realms as well.
Each track meets separately once per month to meet with the leadership and staff of their outpatient continuity clinic to work on practice management and quality improvement. This time is also used for sessions specific to the curriculum of each track: South Campus focuses on border health topics and Alvernon has teaching on integrative medicine topics.
Thursday afternoons are also the time we use for team building, resident support groups, as well as meetings with the chief residents and program director.
Longitudinal Workshops

In addition to general topic reviews there are a set of recurring conferences/workshops including:
- Longitudinal point-of-care ultrasound (POCUS) workshops
- Mock code/emergency scenarios
- Procedure workshops
- Behavioral health
- Board review
- Global/“glocal” health oriented lectures quarterly
- Patient Safety and Quality Conference
- Journal Club
- Adults with intellectual disabilities sessions
- Sports medicine workshops
- Scholarly Project meetings
The Integrative Medicine in Residency (IMR) program is a 150+ hour, competency-based curriculum developed by the Arizona Center for Integrative Medicine with the goal to deliver healing-oriented medicine that takes account of the whole person, including all aspects of lifestyle. It emphasizes the therapeutic relationship between practitioner and patient, is informed by evidence and makes use of all appropriate therapies.
The IMR curriculum covers integrative approaches to prevention and chronic illness management providing evidence-based content in lifestyle medicine and behavioral change, nutrition and dietary supplements, botanical medicine, mind-body approaches, environmental health and manual medicine.
This curriculum is available for both tracks.

To complement the online curriculum, there is dedicated time for on-site integrative medicine teaching and activities:
- Hiking
- Yoga
- Qi gong
- Cooking and hands-on nutrition training
- Motivational interviewing training
- Meditation
- Energy medicine
- Mindfulness activities
- Resiliency training

While all residents obtain training and skills in community health through core curriculum and experiences, our community medicine distinction track allows residents to take a deeper dive into developing skills in delivery of health care to communities with fewer resources, optimizing patient care and health with community resources, and integrating comprehensive knowledge of the factors that impact health outcomes and the promotion of equal health opportunity into the care of our patients.
The primary experience for community medicine distinction track residents is rotating in the Mobile Health Family Medicine Clinic to provide continuity family medicine care through the Mobile Health Program. Additional educational opportunities as part of that clinic experience and residents include developing a scholarly project in community medicine. All residents will rotate through the Mobile Health Family Medicine Clinic, however community medicine distinction track residents will spend additional time, at least once per month, providing care within the clinic.

Preceptors for the Mobile Health Family Medicine clinics are Nicole Person-Rennell, MD, MPH, FAAFP, and Spencer Menapace, DO.

The Global Health Distinction Track provides training to deliver comprehensive, cost-effective and sustainable medical care in underserved areas domestically and abroad. We believe that all people have a right to equitable, culturally responsive health care, and we will continue to advocate for fairness, respect and the advancement of health for all of our patients worldwide.
Program Overview
Predominantly completed during the second and third years of residency, the distinction track offers opportunities to develop expertise in the diagnosis and treatment of common tropical conditions and diseases, and to expand clinical knowledge and management skills in preparation for work in areas of limited resources.
By participating in this program you will be poised to:
- Become a clinical leader in global health dedicated to reducing health disparities in medically underserved communities both in the U.S. and internationally
- Appreciate and experience different cultures and increase cultural awareness
- Apply your experience in different health care systems improving health in all areas of your practice
- Create more awareness about public health in the U.S. and abroad

75% of our Global Health Distinction Track graduates continue to serve globally post-residency.
Curriculum
Monthly global health meetings are organized by second- and third-year residents in the Global Health Distinction Track, and are open to all interested residents.
- Journal clubs
- Resident presentations on their rotations
- Global health case simulations
- Global health book club
- Documentaries
- Current event discussions
Use one of your electives to take the University of Arizona Global Health Course in second year.
- Attended by residents, physicians, nurses, public health students and medical students from North America
- Subjects covered include public health, tropical disease, parasitology, HIV, TB, chronic diseases in international setting, women’s health, child health, epidemiology and numerous other relevant topics
The Quarterly Teaching Day Lecture Series is organized by residents and their global health mentors, and include both resident-led didactic sessions and guest lecturers on topics dedicated to international health.
There are multiple opportunities to participate in trips to the U.S.-Mexico border through organizations such as Borderlinks, Flying Samaritans, Manos de Ayudas and others, and opportunities to work with asylum seekers at Casa Alitas and Kino Border Initiative.
During residents’ third year, they receive sponsored attendance at a global health conference, and all residents have access to an online global health ethics course.
There is a minimum of three weeks of Border/Global Health elective and four weeks of international clinical experience for third-year residents:
- Residents are strongly encouraged to use sites well-known to our university’s global health leaders
- Faculty will help establish contacts and develop the plan and goals for the rotation
Residents also participate in a QI/research project on an approved global health topic:
- Required to present at the Global Health Research Day
- Encouraged to present at a conference
Where in the world are our current partnerships?

- Ecuador
- Nepal
- Northern India
- Argentina
- Zambia
- Vietnam
- Caribbean islands
- Dominican Republic
- Cambodia
- Rural Canada
- Tanzania
- Ghana
- Marshall Islands







Photos from top to bottom, left to right:
Photo 1: Ana Gonzales in the maternity ward, Ghana
Photo 2: Emma Morrow Goodstein
Photo 3: Tricia Wu examining patient in incubator
Photo 4: Hannah Emerson assisting with a C-section, Tanzania
Photo 5: Kela Bergren examining a patient, rural Ecuador
Photo 6: Georgiana Yang leading a mothers education class, Ghana
Photo 7: Maria Ruiz examining a baby, Tanzania
Photo 8: Nasrin Akter listening for fetal heart tones using a fetoscope, Rohingya Refugee Camp, Bangladesh
Photo 9: Several of our residents taking COVID-19 vaccines and antiparasitics to people in rural Ecuador who cannot access them otherwise
Photo 10: Jaylee Caruso in DC advocating for global health education in residency programs through the National Residency Training advocacy coalition
Photo 11: Sommer Aldulaimi
The Spanish Language/Healthcare Disparities Distinction Track is a two-year program that focuses on strengthening the Spanish language skills of residents to enhance the care of our Spanish-speaking patients. We also cultivate discussions and host forums to educate our fellow residents in cultural competency and health care disparities.
Components
- Initial Spanish proficiency testing to determine eligibility
- Continued Spanish proficiency testing to determine progress
- Monthly, one-hour facilitated Spanish classes featuring interactive, systems-based Spanish curriculum
- Access to self-paced Canopy medical Spanish online training modules
- Quarterly health care disparity forums organized by participants featuring local community speakers and topics relevant to the local patient population
- Opportunity to take the ALTA Clinician Cultural and Linguistic Assessment (CCLA) exam and become a certified bilingual provider
- Certificate presented at the end of the two-year distinction track indicating completion and bilingual provider status (if applicable)

Background
There are more than 3 million refugees who have been resettled in the U.S. since 1975, most of whom have fled their country of origin for fear of persecution. Refugees in the U.S. often have histories marked by violence, trauma and substandard living conditions in an intermediate country.
Although refugees are often provided with resources immediately upon arrival the U.S., including case managers, social workers, financial support, housing and help enrolling in services, these services are most often discontinued before the refugees are fully self-sufficient. Arizona is sixth for refugee resettlement in the U.S. and more than 20% of the patients in our two residency clinics are refugees. We have large populations from Somalia, Democratic Republic of the Congo, Rwanda, Eritrea, Ethiopia, the Sudan, Iraq, Syria, Afghanistan, Ukraine, Guatemala and Cuba.
In the U.S., refugees are an underserved patient population who experience significant health disparities and pose unique challenges to the delivery of primary care. Refugees often have limited health care literacy and English proficiency and acculturation issues, along with complex or multiple medical problems, including tropical and infectious diseases and mental health needs. U.S.-trained physicians are often not equipped to deal with these issues in a typical 15-minute office visit. One of our goals is to give residents concentrated time and a curriculum to learn how to care for refugee populations in their future practices.
We have two different clinical experiences involving refugee patients: Refugee Complex Care Clinics and New Refugee Health Screening Clinics. We see refugees of all ages including pregnant patients in both of these clinics.
Refugee Health Curricular Elements
We have several curricular components throughout residency aimed at caring for refugees.
Orientation: Introduction to refugee resettlement and health, and introduction to the care of refugees.
Teaching Days: There are several global health teaching days dedicated to different aspects of care of refugees given by experts in the field. Our colleagues at the refugee resettlement agencies give talks as well.
Clinics: A refugee health-related pearl is done at the start of each clinic on a variety of topics (both health-related and political).
Research: Many residents conduct their Scholarly Projects on refugee-related issues. The complex care clinic originally arose from a resident project.

- Underserved focus in a suburban/urban setting
- Longitudinal integrative medicine experience
ERAS ID: University of Arizona College of Medicine – Tucson Program Alvernon Family Medicine Track
NRMP ID: 1015120C0
ACGME ID: 1200312032

- Underserved focused with rural rotations in Arizona (20 weeks over three years)
- Additional training in emergency adult/pediatric care in under-resourced areas
ERAS ID: University of Arizona College of Medicine – Tucson Program South Campus Family Medicine Track
NRMP ID: 1015120C1
ACGME ID: 1200312032
Apply
Please note that there are two separate tracks affiliated with the University of Arizona Family Medicine Residency Program:
Alvernon Track
ERAS ID: University of Arizona College of Medicine – Tucson Program Alvernon Family Medicine Track
NRMP ID: 1015120C0
ACGME ID: 1200312032
South Campus Track
ERAS ID: University of Arizona College of Medicine – Tucson Program South Campus Family Medicine Track
NRMP ID: 1015120C1
ACGME ID: 1200312032
On top of the salary and benefits that all College of Medicine – Tucson residents receive, Family and Community Medicine residents receive additional benefits:
| NATIONAL CONFERENCE STIPEND | The program supports resident attendance at national conferences as funds are available. |
| MALPRACTICE INSURANCE | Provided |
| MEALS | Meal allowance provided |
| BOOKSTORE & UNIVERSITY EVENTS | Reduced rates; $300 per year, book fund |
| AAFP/AzAFP MEMBERSHIP | Membership paid for all three years while in residency |
| ADDITIONAL BENEFITS | Medical Library access On-Site Gym – available at no cost to residents Lab Coat/Scrub allowance Free parking at hospitals and clinics |
| MOONLIGHTING | Moonlighting opportunities for additional clinical experience and added income are available during third year. State licensure is required. Participation depends on satisfactory performance in the residency, requires specific approval of the Residency Director, and must count towards duty hours per ACGME guidelines. (Request a copy of the policy if interested.) |
For more information regarding salaries and benefits, please access the Office of Graduate Medical Education Housestaff Resources GME webpage.
Resident/Fellow Well-being
The U of A College of Medicine – Tucson is committed to providing resources to support your well-being.
Grand Rounds, Conferences & Events
Learn about events across the college or filter results according to interest.
All About Tucson
Learn about salary and benefits, as well as things to do in Tucson, our desert climate, and the region’s culture.
Meeting Our Mission

Supervised by our faculty, residents rotate through mobile health prenatal and family medicine clinics in a longitudinal fashion throughout residency, providing care to those who have difficulty accessing it.

In partnership with our sports medicine fellows and faculty, residents can volunteer to provide sideline coverage at many school sporting events around the city.

Together, health care providers and lawyers improve the health and well-being of low-income patients and their families. Residents have helped refugees obtain citizenship, families secure better housing, and patients make advanced care planning.
Residents Serving the Community

Naomi Young, MD
Class of 2016 South Campus alum Naomi Young, MD, currently practicing full-spectrum family medicine and serving as chief of staff in her hometown of Ft. Defiance, Arizona, on the Navajo Nation.

Myles Stone, MD
Clas of 2017 South Campus alum Myles Stone, MD, currently practicing full-spectrum family medicine in Tuba City, Arizona, and serving as a member of the U.S. Public Health Service.

Christine Chan, MD
Class of 2019 Alvernon alum Christine Chan, MD, faculty at Hawaii Island Family Medicine Residency.

Patient & Community Advocacy
As part of our residency curriculum and culture, we encourage and educate residents and faculty on the importance of leadership and advocacy for their patients and their communities. This is a thread woven through our clinical and didactic experiences, and enhanced by participation in local, state, and national committees and activities.

Resident Ana Gonzales (second from right) presenting on the First Generation College Student Panel at an event hosted for College of Medicine – Tucson in 2019.

Resident Emma Goodstein (left) presenting Forensic Evaluations for Asylum Seekers: A Skill for Physicians to Advocate for Human Rights at The AAFP Global Health Summit in New Mexico in 2019.

Left: Emma Goodstein, MD, receiving the AAMC ORR Community Service Recognition Award in 2019, given to one resident in the nation across all specialties.
Right: Alumni Shana Semmens, MD, and Myles Stone, MD, giving an International Presentation at WONCA Rural Conference on Palliative Care in Rural Settings in New Mexico in 2019.
Left to right: Residents Josh Blessing, Patricia Wu, Mark Grant and Weston LaGrandeur advocating at the State Capitol for AzAFP Emerging Leaders Day in 2020.

Sommer Aldulaimi and Elizabeth Meehan (faculty) presenting as part of a panel titled “Health Inequities around the World and in the United States: Family Physicians Making a Difference,” at the AAFP National Conference in Kansas City, Missouri, in 2019.

Resident Ricardo Reyes was an invited speaker by members of Guatemalan Acupuncture and Medical Aid Project and Paisanos Unidos (nonprofit organization in Tucson for immigrants). Zoom presentation regarding COVID in Spanish in 2020.
A Medical-Legal Partnership for Health
The Tucson Family Advocacy Program (TFAP) is a partnership of health care providers and lawyers working to improve the health and well-being of low-income patients and their families. TFAP provides free legal services to low-income families in primary care clinics staffed by faculty and residents of the Department of Family and Community Medicine. Within these medical settings, TFAP also teaches health care providers about legal issues that impact health and how they can become more effective advocates for their patients. By combining the unique strengths of multiple professions — law, medicine, pharmacy and social work — TFAP helps families obtain the services they need to prevent or resolve crises that undermine health.

Resident Scholarly Activity, RSPP and QuIPS
Residents from both our Alvernon Track and South Campus Track are required to participate in scholarship. We meet these requirements through our Resident Scholarly Project Program and Quality Improvement and Patient Safety presentations.
Resident Scholarly Project Program (RSPP)
The Resident Scholarly Project Program involves collaboration with a clinical mentor and research mentor to develop and answer a research question through a process of critical inquiry. RSPP starts in the middle of PGY1 with the identification of a topic area and mentor matching. It concludes at the end of the third year with a departmental presentation, as well as encouragement and support for presentations at regional and national conferences and peer-reviewed publications.
If you have questions, please contact the RSPP co-directors, Yumi Shirai, PhD, and Allison Huff, DHEd, at RSPP@arizona.edu.
Quality Improvement and Patient Safety (QuIPS)
The Quality Improvement and Patient Safety Conference is led by Karissa Wasiak, MD. QuIPS is a longitudinal educational experience with the goal of engaging residents in quality improvement and patient safety work within clinical systems. QuIPS emphasizes systems thinking, interprofessional collaboration and the identification of modifiable contributors to adverse outcomes or near misses. Residents lead one QuIPS session per year in groups of four, selecting and presenting real, de-identified clinical cases, often ones in which they were directly involved. By leading a structured discussion that explore contributing factors, areas for improvement and opportunities for change are identified. The program fosters a culture of psychological safety, empathy and continuous improvement rather than blame.
2025
- Color, Calm, and Care: Visual Art in Healing Spaces Jessica Pirkle
- A Mind-Body Medicine Movement and Meditation Experience for Residents Benjamin Lombardo
- From Dust You Come, and Unto Dust You Return Nicholas Ahern
- Primary Care is Community Anna Moga & Radu Moga
- Prenatal Outcomes Evaluation in the Mobile Health Program Chloe Kidd and Hannah Emerson
- Effects of 5-Needle Auricular Acupuncture on Healthcare Worker Burnout Jaylee Caruso & Kevin Ruaro
- Effects of MOUD Training Experiences Among Primary Care Residents on Likelihood to Manage Future OUD Patients with Buprenorphine vs Methadone Robert Woodruff
- The Collection and Use of Pronouns in Healthcare Settings Jinx Lioi
- Exploration of the Relationship between Food Insecurity and Mental Health in Pediatric Student Athletes Rachel Baca, Stephanie Jones, & Danielle Kulpins
2024
- Enhancing Medical Education through a Resident-Led Art Medical Humanities Project Alex Lim, Kevin Ruaro, & Rahotep Alkebulan
- Concusion Protocol for Alvernon Clinic Michelle Do & Jason Dorian
- Barriers to Discharge at Banner South Hospital Carli Ogle & Colleen Sells
- From Responders to Partners: Enhancing Outpatient Services Cynthia Sanchez
- Advanced Care Planning and Refugees Daniel Anderson, Taylor Buel, Bryce Hunsaker, Megan Garrett, Amanda McKeith, DJ Murphy, & Georgiana Yang
- Confidence in IUD Placement in Male vs Female Residents Bernardo Chavira
2023
- Inner Light and Inner Strength Sameer Suhale
- (Medicine) A Placeholder Joan Tran
- Ten Jessica Filon
- Residency in the Time of COVID-19 Ricardo Reyes
- Have Burnout? Do NADA! Abigail Stephens & Nikie Tong
- UA Breastfeeding and Lactation Policy for Medical Trainees Jennifer Stepp
- Assessing Food Insecurity Awareness in Family Medicine Residents Jennifer Akazawa
- Concussion Protocol for Alvernon Clinic Jason Dorian & Michelle Do
- Refractory Ankle Pain: A Case of Septic Arthritis Kareem Shahin
2022
- Painting – Fatima Giron Rivas
- Song: Arrhythmias in Motion Drum and Bass – Francisco Gomez & Sean McEvoy
- Film Documentary: Behind the Mask – Daniel Luccock & Karissa Wasiak
- Poem: ICU Bed 14 – Natasha Mitra
- Painting: Beautiful Chaos II – Natondra Powell
- Painting: Disconnect – Kela Bergren
- AZ PCP Pocket Guide to Palliative Care – Rachel Bruckman
- Painting: Bloom On – Clare Donahue
- Research Poster: MJ and Breastfeeding –Caroline Flowers
- Song: Goodnight – Justin Gause
- Poem – Mark Grant
- Painting – Marisela Mariscal
- Song: Kino Hospital – Hadley Pope
2021
- Lights in the Darkness – Ambereen Ahmed
- My Love Letter to Family Medicine – Nicolette Barbour
- A Spectrum of Emotion – Bryan Brown
- Beyond the "See" – Jeiran Javaherian
- Layers of Emotion – Jennifer Veaco
- Hurt – Joey Harkins, Javier Laguillo
- Flow – Connie Herrera
- All the Things We Think We Know – Sean Maiolo
- Decreasing Healthcare Disparities by Increasing Resident Involvement in Free Clinics – Weston LaGrandeur
2020
- A Scoping Review on the Effect of Pre-Residency Preparation on Intern Preparedness, Authors: Harris, Shima
- The Healthy Self Project Evaluation of Utility of Mind-Body Therapies for Stress Management in High School Students, Authors: Kumala
- Will Identifying and tailoring a traditional Somali diet improve glycemic control in diabetic patients, Authors: Ahmed, Jean
- A Comparison On How Frequently Important Diagnoses Are Seen Across the Nation. Authors: Sayre, Sipos
- Medical Staff and Provider Opinions on Expanding Clinic Hours. Author: Blessing
2019
- Increasing Resident Comfort in Assessing Fall Risk: An EMR-based Intervention, Authors: Lecture, Armin, Howe
- Expanding Access to Point of Care Ultrasound (POCUS) in Primary Care, Author: Gadzik
- ED High-Utilizers: Resident Attitudes, Experiences, and Motivations to Affect Change, Author: Chan
- Are providers asking men about their sexual health?, Author: Setareh
- Cervical Cancer Screening Rates in Refugee and Non-Refugee Patients, Author: Grigsby
- Resident Impressions of the Clinic Experience: Impact of the 2+2 Model, Author: Hartl
2018
- Arizona Lifestyle Inventory Effect on Wellbeing in Medical Students. Author: Howard
- Care Transitions for Homeless Patients. Author: Garcia
- Developing A Wellness Program for Patients with or at risk Type 2 Diabetes. Authors: Ford, Clark
- Dramatically Increasing Youth Immunization Against HPV and Influenza Using Video Clips. Authors: Huynh, Chan
- Banner Clinical Practice: Rhabdomyolysis Presentation. Author: Sprague
- The Effect of Treadmill Desks on Physician Efficiency. Author: Schatz
- Hepatitis B vaccine in non immunized adults. Authors: Jenny Saint Aubyn MD, Tiffany Castellano MD
- Utility of Routine Prenatal Urine Dipsticks. Authors: Michele Alba, MD and Zoë Cappe, MD
- Pre-Implementation Evaluation of Nursing Patient Acuity Tools (PAT). Authors: Todd A. Horstman, MD, Marcos A. Teran, MD
- Refugee Health: Creating a clinic model for the successful integration of refugees into the U.S. healthcare system. Authors: K. Losey; T. Castellano; A. Mendez; J. Saint Aubyn; P. Wang; J. Koleski; S. Aldulaimi
2017
- Sleep In-Equality. Authors: Bailey, Parthasarathy, Ojo, Garcia
- Just Another Reason to Dislike LAX... Author: Singer
- Transition to Medical School: Assets and gaps in resources identified by PreMedical Admissions Pathway students. Authors: Selpid
- Point of Care Ultrasound: Development of a Resident-led Family Medicine Curriculum. Authors: Carrasco, Raub, Moran
- Improving Communication with Limited English Speaking Patients in a Resident Clinic. Authors: Bitow, Armin, Moran
- Implementation of Food Insecurity Screening for Pediatric Patients in a Family Medicine Clinic. Authors: Akazawa, Martineau, Ric
- Gaps in Quality Measures Among COPD Patients at the Alvernon Family Medicine Residency Clinic. Authors: Selpides, Ricker
- ACT! Advanced Contracepton Training A model to increase family planning discussions in a resident clinic. Authors: Grace Price, MD and Shana Semmens, MD
- USPSTF Screening Guideline Table: Improving Screening and Teaching. Author: Joshua Clutter, MD
- Physical Therapy Expectations and quality Measures in Acute and Chronic Musculoskeletal conditions. Authors: J.Anthony Saenz, MD, Patrick J Goetz, MD, Jason Patel, MD, and Sommer Aldulaimi, MD
- Comparison of Methods Used to Detect Insulin Resistance in Overweight and Obese Children. Authors: Katie Houmes MD, Randa Kutob MD, MPH, Chris Ussery, MS, Kathylynn Saboda, MS, Scott Going, PhD, Denise Roe DrPH, Craig Stump MD, PhD, Melanie Hingle, PhD, MPH, RD
- Refugee Clinic at South Campus – What we have learned so far. A clinic within a clinic to improve the standard of care for refugee patents. Author: Shana Semmens, MD
- Non-communicable disease evaluation as the basis for primary care improvement in the Nam Giang district of central Viet Nam. Authors: Myles Stone, MD, MPH, Hy Sy Quang, MD, Matthias Huber, Joshua Solomon, MD
2016
- Why Do Low Income Patients Use Tobacco? A Mixed-Methods Study. Authors: Bradley, Yang, Desai, Gordon
- Recruitment Strategies Used in a YMCA-Based Intervention to Prevent Type II Diabetes in At-Risk Youth. Authors: Soliz, Olkiewicz
- Post-Partum Contraception Methods in Alvernon FMC OB Patients. Authors: Quigley, Richardson, Moran
- Marijuana and its Cardiovascular Effects: A Systematic Review. Authors: Reynolds, Clements
- Improving the Cultural Competency of Medical Students in Working with LGBT Patients through an Enrichment Elective. Author: Nguy
- Diabetes Education in Our Clinic: Does it Stick? Authors: Cynthia Carrillo, MD; Chantelle Chen, MD; Daphne Rosales, MD; Mary Harrel, MD
- At What Age is Aggressive Intervention Recommended to Prevent Obesity In American Indian/Alaska Native Children? Authors: Madeline Sanchez, MD, Naomi J Young, MD, Francine Gachupin, PhD
- Refugee Health: Creating a clinic model for the successful integration of refugees into the U.S. healthcare system. Authors: Lori H Landes, Tiffany Castellano, Kaitlyn R Losey, Ana M Mendez, Jenny F Saint Aubyn, Jerome F Koleski, Sommer Aldulaimi, Susan K Hadley
2015
- Advance Directives Residency Curriculum. Authors: Wofford, Becerra, J. Gordon, and Anne Ryan
- Back to Basics: Does Focusing on the Fundatmentals of Energy Medicine Increase Receptivity? Authors: Artrip and Sandal
- Dermascopy to Improve Family Medicine Residents' Diagnostic Accuracy of Skin Lesions. Authors: Riebe, Olkiewicz, Soliz, and P. G.
- End of Life Discussion with Persons with Disabilities Authors: Pham, Le, and Tomasa
- Improving Resident Confidence and Competency for Well Child Visits from Infancy to Two Years of Age. Author: Riebe
- Case-Based Learning in Family Medicine Residency Training. Authors: Megan M. Rayman, MD, Joie L. Evans, DO, Karyn Kolman, MD, Judith Gordon, PhD.
- Common Factors Affecting Therapeutic Non-Compliance: A Systematic Review. Authors: Bea Piña, MD; Allison Hopkins, PhD.
- Cost Acknowledgement Decreases Test Ordering in Physicians. Authors: Paul F Swenson MD, Benjamin A Gonzalez MD, Ahlam A Saleh MD MLS, Daniel J Derksen MD.
- Educating Providers on Effective Healthcare for Adults with Intellectual and Developmental Disabilities. Authors: Jessica Hensel, MD, Leslie Cohen, JD, Tamsen Bassford, MD, Sarah Guayante.
- Hypertension Prevalence Among an Ethnically Diverse Patient Population in a Southwest Medical Network. Authors: Victoria McCurry, MD, Allison Hopkins, PhD.
- USPSTF Recommendation Schedule: A novel teaching tool for preventative medicine teaching. Authors: Paul F Swenson MD, Coya Lindberg MD, Cynthia Carrillo MD, Joshua Clutter MD.
2014
- Does Readiness to Exercise Predict Weight Loss Success in a Lifestyle Modification Program? Authors: Crowe and Sozanski
- Designing a Global Health Curriculum in a Family Medicine Residency. Authors: Moran and Johnston
- Prevention and Wellness: An Online Elective for Medical Students. Authors: Horzempa and Salomon
- Using a Patient Focused Approach to Aid in Smoking Cessation. Author: Yaqub
- Thrush in the Breastfeeding Dyad. Author: Khalife
- Use of Weight Positive Medications in Obese or Overweight Patients with Chronic Conditions. Authors: Olivas, Bera, Muramoto
- Attitudes, Self-Efficacy, and Perceived Barriers Toward Diagnosing, Preventing and Treating Obesity in the Primary Care Clinic. Authors: Amanda R. Marquis, MD1, Judith S. Gordon1, PhD, Cynthia Thomson, PhD.
- Mobile Health Program Group Prenatal Care and Pregnancy Outcomes. Authors: Palitha Kalpage MD,MPH and Allison Hopkins PhD.
2013
- Expanding the Toolbox of Obesity Prevention Measures. Author: Byron
- Text Messaging Based Smoking Cessation - Resident Physician's Knowledge and Beliefs. Author: Firth
- Healing Burnout in Residency. Authors: Grund, DeLiere, Lebensohn
- Evaluating Barriers to Healthcare Among Patients with Visual and Hearing Impairments. Authors: Pham Haase and Ritter
- Evaluation of Literacy Among Refugee Patients and Subsequent Effect of Providing Books. Authors: Lokale and Lebensohn
2012
- Is Showing Up Really 50% of the Job? Targeting Success for Weight Loss. Author: Dake
- Acupuncture and Smoking Cessation Studies. Author: Kauffman
- Impact of Biweekly Group Education on Dietary Habits of Populations at Risk for Diabetes II. Authors: Leano, Sonneborn, Kutob
- Evaluation of the Patient with a Suspected Deep Vein Thrombosis (DVT) in an Outpatient Setting. Authors: Trieu and Hicks
- Making Group Visits Financially Feasible for Diabetics and Pre-Diabetics. Author: Uselman
- Reasons for Smoking in a Low-Income Population: A Qualitative Study. Authors: Yang, Desai, J. Gordon
- Resident Attitudes & Practices in the Care of Adult Sexual Assault Patients in Tucson, AZ. Author: Guffey
- Lipid Lowering Therapy in Diabetics. Authors: Ramakrishnan and Cagno
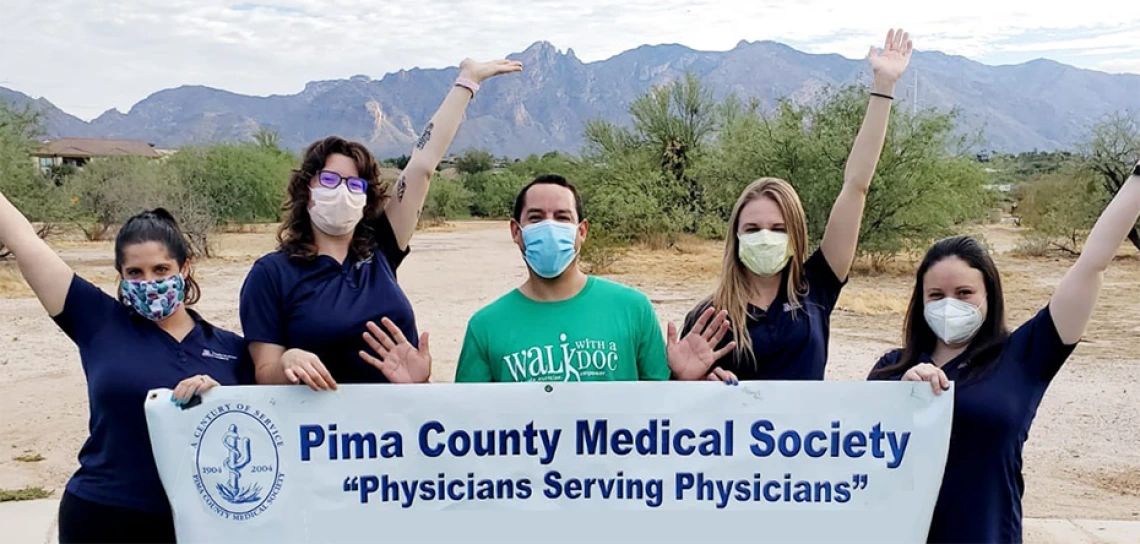
Community Involvement


Community involvement events
- Docs on Bikes
- Walk with a Doc
- Health fairs
- Pathways to success high school fair
- Free sports physicals
- Opportunity to be a high school football team doc
- Pima County Health Department
- Home visits
- Casa Alitas (asylum seeker clinic)
- Opportunity to get certified to do medical forensic exams for asylum seekers
Visiting Student Scholarship
- Encourage students who self-identify with groups that are underrepresented in medicine to consider residency at the University of Arizona College of Medicine – Tucson
- Promote student awareness of opportunities in academic medicine
- Provide mentoring and networking for students who identify as underrepresented in medicine
- Provide a stipend of up to $1,500 to help offset cost of housing and travel
Karyn Kolman, MD
Program Director
kbkolman@arizona.edu
520-621-6323